Breastfeeding
Breastfeeding Centre (BFC) Classes
The Breastfeeding Centre runs the following online classes with Lactation Consultants IBCLC (International Board-Certified Lactation Consultants). These classes are open to public patients across the state.
- Antenatal preparation for breastfeeding
- Helping your baby to breastfeed
- Breastfeeding and diabetes
King Edward Memorial Hospital (KEMH) is a Baby Friendly Health Initiative (BFHI) Accredited Hospital where a mother's informed choice of infant feeding is encouraged, respected and supported.
There are a variety of ways that women can access breastfeeding information and breastfeeding assistance here at Women and Newborn Health Service (WNHS).
Our parent education department run breastfeeding workshops for women who have their baby at WNHS.
Women with complex needs can access a one-on-one appointment at the Breastfeeding Centre. Ask your midwife for more information.
In Australia, overseas visitors, overseas students and patients who are not eligible for Medicare under their current VISA arrangements are required to pay for the cost of their health care. Please contact the Overseas Liaison Officer on (08) 6458 1066 or email KEMHPPLO@health.wa.gov.au to obtain information regarding fees for your appointment.
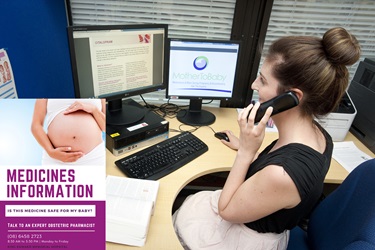
Medicine Information line
The Obstetric Medicines Information Service at WNHS provides mothers, families and health professionals information about the safe use of medicines during pregnancy and when breastfeeding.
The Medication Safety Line is available on (08) 6458 2723 and provides information to women anywhere across Western Australia between 8.30am and 5pm Monday to Friday. Women, unsure of the effects of medication either prescribed or over the counter, can call to receive reassurance from qualified Pharmacists.
Often uncertain about the safety of taking medications during pregnancy and breastfeeding, the line provides an enormously valuable resource for WA Women.
Medicines information in pregnancy and breastfeeding - helpline (PDF)
Medicines and breastfeeding
The importance of breastfeeding is well recognised with benefits for both the mother and infant. Breast milk provides babies with unique nutrients that are ideal for their immune protection, growth and development.
Many breastfeeding mothers need to be treated with medicines, either for a chronic illness requiring ongoing therapy or for an acute illness requiring only a few days therapy. Some mothers stop breastfeeding while taking medications to treat these conditions because of unfounded concern or inappropriate advice.
It is widely accepted that medications transfer into human milk to some degree, although the amount is generally quite low and this is why most medicines are considered safe to take while breastfeeding. Only rarely does the amount transferred into breastmilk produce clinically relevant doses in the infant.
The safety of breastfeeding while a mother is taking a medication may be assessed by weighing the risks of potential adverse effects in the baby, against the benefits of the medicine for the mother and the benefits of breastfeeding for the baby and mother.
Minimising transfer of medications into breastmilk
- Avoid using medicines unless they are necessary.
- Your doctor will prescribe the lowest dose for your condition.
- Think of ways to choose a dose that reduces how much is passed into breastmilk e.g. use a decongestant nasal spray rather than an oral decongestant.
- To reduce the amount of medicine in the breastmilk, time your feed eg. taking a dose immediately after a feed, or before baby’s longest sleep period.
Important information
When taking any medicine, watch for signs of possible side effects in your baby such as increased sleepiness, poor feeding, rash and severe diarrhoea.
If these are troublesome and continued, contact your doctor
Always ask your pharmacist what is in a medicine and tell them you are breastfeeding.
Commonly used medications
Aches and pain - analgesics
- Non-steroidal anti-inflammatory medicines (NSAIDs) like ibuprofen or diclofenac have low transfer to breast milk and are considered safe to use to relieve pain and inflammation.
- Paracetamol can be used safely during breastfeeding to treat mild pain or reduce fever.
- Low doses of aspirin, less than 150mg daily, are considered safe to take. Larger doses should be avoided as they may be harmful to your breastfed infant.
- Medications containing codeine
Medications containing codeine are no longer recommended for pain relief in breastfeeding mothers.
Codeine metabolises to morphine in the body and a small number of people produce higher than expected morphine levels in their blood resulting in an increased risk of transfer to the infant via the breastmilk. Alternative pain control medicines as mentioned above are recommended.
Cold and flu
Body aches and pain – see above (analgesics)
Nasal symptoms
- Steams inhalations and saline (sodium chloride) nasal spray may be used to relieve a blocked nose while breastfeeding.
- Decongestant nasal sprays (oxymetazoline, xylometazoline) may be used for 3 to 5 days.
- Avoid oral preparations containing pseudoephedrine as it may reduce milk production or cause irritability in a breastfed baby.
Cough
- A cough is usually self-limiting. If treatment is required, use guaifenesin, bromhexine or senega and ammonia mixture for a chesty cough.
- A cough suppressant like dextromethorphan is considered safe for a dry cough. Avoid combination preparations containing pseudoephedrine and phenylephrine – always ask your pharmacist what is in a medicine.
Sore throat
- Lozenges or throat gargles containing local anaesthetic, antibacterial agents or benzydamine may be used while breastfeeding.
- Avoid products containing povidone-iodine (e.g. Betadine®) as it may affect the thyroid function of your baby.
Allergies and hay fever - antihistamines
- Non-drowsy antihistamines such as loratadine, desloratadine and fexofenadine are present in very small amounts in breastmilk and are considered safe to use whilst breastfeeding. Drowsy antihistamines such as cetirizine, dexchlorpheniramine or diphenhydramine may make your baby drowsy, so less sedating antihistamines are preferred.
- Nasal sprays containing beclomethasone, fluticasone or budesonide may be used while breastfeeding. Topical eyedrops for allergies and hay fever may be used as the amount transferred into breastmilk is low. Eye drops containing antazoline and naphazoline are considered safe to use.
Anti-infectives
Which antibiotics are safe?
Most antibiotics transfer into breastmilk, but the amount ingested by an infant is unlikely to cause serious harmful effects. However some antibiotics can cause changes in gut bacteria and infants should be observed for adverse effects such as diarrhoea, vomiting, skin rashes or thrush.
Penicillin antibiotics (including amoxicillin, amoxicillin with clavulanate and flucloxacillin), cefalexin, erythromycin and azithromycin are considered safe. Metronidazole is considered safe in doses up to 400mg three times a day, although it may give the milk a bitter taste.
What can I use to treat worm infections?
Both pyrantel and mebendazole are considered safe as they are poorly absorbed from the gut and are unlikely to be passed into breast milk in clinically relevant amounts.
What can I use for vaginal thrush?
Topical antifungal cream and pessaries containing clotrimazole, miconazole and nystatin are safe to use while breastfeeding.
A single dose of oral fluconazole is considered safe to use whilst breastfeeding.
What can be used to treat cold sores?
Ice is a recommended treatment which can be applied to the affected area.
Antiviral medicines such as aciclovir cream can be used in breastfeeding, and if the cold sores are severe an oral course of aciclovir or valaciclovir from your doctor would be considered safe to use whilst breastfeeding. These options are preferred to famciclovir which has no published data on how much enters breastmilk.
Head lice
Non-insecticidal treatment ─ 10 days hair conditioner method: Apply plenty of hair conditioner to the dry hair until saturated, use ordinary comb to remove tangles, then use metal fine tooth nit comb in 4 directions (forward, backward, left and right). Remove lice from comb. Rinse out and dry hair. Repeat every 1 to 2 days over a 10-day treatment period.
Insecticidal treatment – Permethrin, Dimeticone or pyrethrin / piperonyl butoxide can also be used if needed. Treatment should be repeated in 7 days to kill lice that have hatched.
Flu vaccine
Breastfeeding mothers may continue to breastfeed after immunisation with flu (influenza) vaccine.
COVID-19 vaccines
The Comirnaty Pfizer®, SpikeVax Moderna® and Nuvaxovid NovaVax® vaccines are considered safe to be used whilst breastfeeding. These vaccines are recommended for women who are breastfeeding. You can continue breastfeeding before or after your vaccination.
Antidepressants
Some antidepressants are considered compatible with breastfeeding. Talk to your doctor or pharmacist to discuss your options and for further advice.
Herbal preparations
There is very little information available on the distribution of herbal preparations into breast milk, or their effects on lactation. Care should be exercised with their use. Talk to your doctor or pharmacist to discuss your options and for further advice.
Oral contraceptives
The progesterone-only “minipill” is the preferred oral contraceptive for breastfeeding women as transfer to milk is minimal and lactation is not affected.
The combined estrogen-progesterone pill may decrease the quantity and alter the composition of breastmilk. It may be considered after 6 weeks if breastfeeding is well established.
Overseas patient fees
Hospital fees for patients who are not eligible for Medicare are set by the WA Department of Health. Overseas visitors and overseas students are required to pay for the cost of their care. Calls made to the Maternal Fetal Assessment Unit (MFAU) by Medicare ineligible patients, such as overseas visitors and overseas students, will incur a charge.
More information about overseas patient fees.





